Researching what is clinically needed
In scientific research in the field of epilepsy, Kempenhaeghe has built up a broad ‘repertoire’. In the past twenty years a range of subjects has been studied and many steps, sometimes little, were taken. These steps have helped professionals to establish a better diagnosis and further improve the treatment of people with epilepsy. One of the outcomes is the option to consider drug-free treatment methods at an earlier stage.
Kempenhaeghe’s ‘good practice’ to link clinicians with technicians in scientific research started in epilepsy research projects. Clinicians and technicians work together on research questions that result from the daily care practice. Results are embedded there. Starting point is always what is clinically needed, rather than what is technically possible. Goal is to find a better perspective for research and treatment of patients in order to improve their quality of life. The current scientific activities of the Academic Center for Epileptology focus in particularly on:

Seizure detection: Safety in epilepsy
Despite treatment a major part of people with epilepsy suffer from seizures. This can – especially at night – lead to dangerous and sometimes life-threatening situations. The proximity of a loved one can help limit the risk of seizures. But nightly seizures often remain unnoticed. That is why it is important to deploy a reliable type of seizure detection.
Initiated by neurologist prof. dr. Johan Arends (recently retired) a broad cooperation – the so-called Tele-epilepsy consortium – was established with the Academic Center for Epileptology at Kempenhaeghe and Maastricht UMC+, the University of Technology Eindhoven, epilepsy center SEIN, UMC Utrecht, LivAssured and representatives of patient organizations. Together, these parties work under the direction of neurologist Richard Lazeron, on methods to safely detect seizures.
Medication: Choosing the best medication
When someone turns out to have epilepsy, medication is usually selected as the first treatment method. There are guidelines to support the neurologist in his choice of medication. These guidelines suffice for most, but not all patients. That is why it remains necessary to improve existing treatments or develop new ones.
Most epilepsy patients benefit from the medication prescribed by the neurologist in the first or second instance. In patients who come to Kempenhaeghe it has often been impossible to become seizure-free with medication, as determining the right medication is complex in this group of patients. Many of them use a combination of medicines: sometimes multiple AED’s, but also AED’s and medication for other disorders. It is important to keep the expertise on choice, use, side effects, interaction and cost effectivity of AED’s up-to-date and share this information.
That is why we engage in scientific research, for instance by contributing our expertise in pharmaceutical studies initiated by pharmacists. Our pharmaceutical research group consists of doctors, behavioral scientists, research nurses and specialists from our pharmacy and laboratory. The group works on projects on specific diets, on side effects of AED’s and on the early selection of the best suitable AED for a patient.
Genetics research: Finding the cause for tailormade solutions
Epilepsy can have genetic causes. If this is suspected or established, Kempenhaeghe brings in a clinical geneticist to perform DNA-tests. The findings from these tests can give direction to the treatment. Symptoms, the progress of the clinical picture and possible consequences for (future) children and other family members, can possibly be explained better.
At this moment 300 genes are known that are involved in epilepsy. Genes are pieces of DNA that determine the genetic properties of a person. It is important to obtain more know-how on this. That is why we engage in scientific research.

Epilepsy surgery: Exactly defining the operation area
When anti-epileptics do not stop the epileptic seizures or have undesirable side effects, we examine whether epilepsy surgery could be an option for the patient. The focal question is whether the epileptic seizures originate in a definable area in the brain and whether this area can be removed without considerable damage to the patient. The more precise the area can be defined, the bigger the chance of a successful surgical procedure.
An important part of the scientific research of the Academic Center for Epileptology, in cooperation with other academic parties and SEIN, focuses on being able to pinpoint and define the source of epilepsy. In the past years, considerable progress has been made and thus, more patients qualify faster for epilepsy surgery.
Neuro-imaging: picturing the brain networks
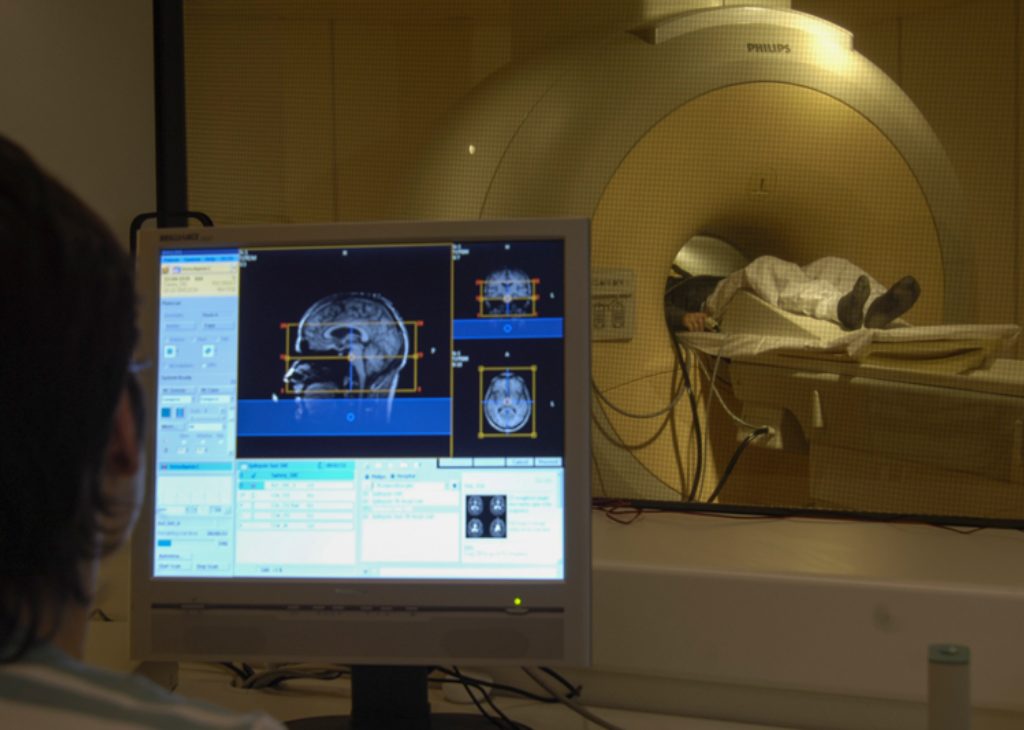
Imaging techniques are a great ‘present’ in care. They are non-invasive and enable finding deviations that previously remained unseen. Whereas much is possible, at the same time there is a great need for improvement and innovation. Part of the scientific research at Kempenhaeghe focuses on imaging the effects of epilepsy, in particular the cognitive effects, on brain networks, and making the dynamics of epileptic seizure sources visible. There is a great deal of benefit to be had here. Kempenhaeghe’s own MRI is an indispensable facility in this research field.
Our scientific projects in the field of neuro-imaging are largely embedded in the broad research consortium Neu3Ca, in which Kempenhaeghe, the University of Technology, Maastricht Universitair Medisch Centrum and the Universitair Ziekenhuis Gent cooperate with other knowledge centers and industrial parties. The consortium is supported by the European Institute for Innovation and Technology (EIT-Health). Neuro-imaging is one of Neu3Ca’s three research fields, the other ones being neurostimulation and neurodegeneration. As a result of this cooperation we literally obtain an increasingly better image of the brain. Within neuro-imaging we are constantly looking at changes in the brain in functional areas. In time, this will result in better and more targeted therapies.